150
Проблемы биологии и медицины, 2014, №4.1 (81)
UDC: 621. 316. 9. 612. 015. 348. 616-089. 811
PROTECTIVE EFFECT OF L-ARGININE ON HEPATIC ISCHEMIA REPERFUSION INJURY:
AN EXPERIMENTAL STUDY
O. OLESHCHUK
HSEI “I.Ya. Gorbachevsky Ternopil State Medical University of Ministry
of Public Health of Ukraine”
Resume.
A major problem complicating liver transplantation is the preservation injury that results
from ischemia/reperfusion (I/R) injury after organ revascularization. The L-arginine-nitric oxide (NO)
pathway has been recognized to play critical roles during organ injury and transplant rejection. Recent data
indicates that NO synthesis has beneficial effects in several models of liver injury. The purpose of this
study is to examine the role of L-arginine on preservation injury in an experimental model of rat I/R.
Methods: Complete ischemia of the median and left hepatic lobes was produced by clamping the left
branches of the portal vein and the hepatic artery for
45
min., than 2 h of reperfusion. Rats were pre-
cotreated with L-arginine (25 mg/kg i.p.) for 3 days before, last time 10min before induced ischemia-
reperfusion maneuver. Results: L-Arginine supplementation provided activation of a constitutive form of
NO-synthase, thereby inducible NOS activity decreased, but remained its significantly higher than that of
the control. L-Arginine influences also on the level of proinflammatory cytokines, and the content of IL-
1β, IL-6 and TNF-α were decreased. Also L-Arginine decreased hepatic transaminase levels at the time of
examination. Conclusions: The results show that L-arginine supplementation and NO synthesis improve
hepatic injury and have a protective role in the I/R injury. The enhanced production of NO through the
administration of L-arginine balanced NO-arginine system, proinflamantory cytokine profile, protect liver
at I/R induced injury. The protective effect may be mediated by activation of cNOS-derived NO.
Key words:
L-arginine, hepatic ischemia reperfusion.
ЗАЩИТНЫЙ ЭФФЕКТ L-АРГИНИНА НА ПЕЧЕНОЧНУЮ ИШЕМИЮ
РЕПЕРФУЗИОННОГО ПОВРЕЖДЕНИЯ: ЭКСПЕРИМЕНТАЛЬНОЕ ИССЛЕДОВАНИЕ
О. ОЛЕЩУК
ГВУЗ «Тернопольский Государственный медицинский университет
им. И.Я. Горбачевского МЗ Украины»
Резюме.
Основная проблема осложняет трансплантацию печени травмы сохранение, что
приводит к ишемии / реперфузии (I / R) травму после органной реваскуляризации.L-аргинин-оксид
азота (NO) путь был признан играют важную роль в процессе повреждения органов и отторжение
трансплантата. Последние данные показывают, что NO синтеза не имеет положительный эффект в
нескольких моделях повреждения печени.Целью данного исследования является изучение роли L-
аргинина на травмы сохранения в экспериментальной модели крыс I / R. Методы: Полный ишемия
медианы и левой долей печени было произведено путем закрепления левые ветви воротной вены и
печеночной артерии в течение 45 мин, чем 2 ч реперфузии. Крысам было предварительно введено
L-аргинин (25 мг / кг внутрибрюшинно) в течение 3 дней прежде, последний раз 10 мин до
индуцированной ишемии-реперфузии маневра. Результаты: L-аргинина, предусмотренные
активацию конститутивного виде NO-синтазы, таким образом, индуцируемый активность NOS
уменьшилась, но оставалась его значительно выше, чем у контрольной группы. L-аргинин влияет
также на уровне провоспалительных цитокинов и содержание IL-1β, IL-6 и TNF-α были снижены.
Также L-аргинин уменьшилось печеночных трансаминаз в момент обследования. Выводы:
результаты показывают, что добавление L-аргинин и NO синтез улучшить повреждения печени и
имеют защитную роль в травму I / R.Усиливается производство NO путем введения L-аргинина
сбалансированный NO-аргинина системы, воспалительный профиль цитокинов, защитить печень
вызванной травмой. Защитный эффект может быть опосредована активацией CNOS-производного
NO.
Ключевые слова:
L-аргинин, печеночная ишемия, реперфузия.
Inroduction.
Ischemia-reperfusion (I/R)
liver injury occurs when blood flow is restored after
prolonged ischemia. This is a phenomenon whereby
cellular damage occurs because of oxygen delivery
into the liver tissue. This form of injury in the liver
was
recognized
as
a
clinically
important
pathological disorder [1]. Liver injury caused by I/R
occurs in various surgical interventions, including

O. Oleshchuk
Биология ва тиббиёт муаммолари, 2014, №4.1 (81)
151
hepatectomy and liver transplantation [2]. I/R injury
is associated with an acute inflammatory response
and microvascular dysfunction, which finally lead to
irreversible cell injury [3].
The pathogenesis of liver damage during
transplantation, as an example of
I/R
, is very
complex and occurs in two stages; the initial injury
is caused by ischemia but aggravated further by
reperfusion of the organ. I/R injury in the liver
involves an early acute phase, associated with the
generation of free radicals and nitric oxide (NO),
and with T-lymphocyte and Kupffer cell activation,
followed by a subacute phase, characterized by
neutrophil infiltration leading to continued oxidant,
cytokine, and chemokine production [4,5].
Since the discovery of nitric oxide (NO)
about 30 years ago, the field of NO research has
been rapidly expanding and new aspects of NO
activity continue to emerge. L-Arginine is the
substrate constitutive and inducible NOS and
arginase for the production of NO and urea,
respectively [6]. In mammals, α-amino acid arginine
is classified as a semiessential or conditionally
essential
amino
acid,
depending
on
the
developmental stage and health status of the
individual. The L-form is one of the 20 most
common natural amino acids [7]. Nitric oxide (NO)
– a potent vasodilator, that diffuses freely across cell
membranes and acts intracellularly by the activation
of guanylate cyclase. NO is an inducer of
vasodilatation at the level of the sinusoid as well as
at presinusoidal sites [8]. In addition to its
vasodilatory effect, NO reacts with superoxide to
form the potent oxidant peroxynitrite [ 9]. NO
inducer of vasodilatation at the site of sinusoid as
well as at presinusoidal sites[ 10,11], which causes
vasodilatation in Kupffer cells. NO also reacts with
superoxide to form the potent oxidant peroxynitrite
[12]. Inducible nitric oxide synthase (iNOS) from
hepatocytes activates Kupffer cells to produce nitric
oxide (NO). We, as some other scientists,
hypothesized that the modulation of vasodilatation
by NO could explain the protective effects of liver
from I/R induced injury [13].
The effect of L-arginine therapy on hepatic
ischemia has not yet been completely elucidated.
Therefore, it was decided to investigate the role of
nitric oxide donor L-arginine in I/R-induced injury,
and the present study was designed to ascertain
whether differences in the production of NO by
hepatocytes cells could explain the differences in
liver state found in I/R injury. Further pathological
changes in the different experimental and sham-
operated control groups were correlated with
histopathology study.
Materials and methods:
L-arginine were
procured from Sigma; Alanine aminotransferase
(ALT) and Aspartate aminotransferase (AST) Kits
were procured from “Filisit-Diagnisric”; TNF-α, IL-
1β, IL-6, eNOS, and iNOS ELISA Kits were
procured “Uscn limited inc”.
Animal model.
Male white
rats (Ternopil
state medical university vivarium, Ukraine)
8-10
week old, weight 300-350 g, were used in these
experiments. All animals were fasted 12 h before
experimentation and allowed water ad libitum. All
animal received care in compliance with the Guide
for the Care and Use of Laboratory Animals
(National Institutes of Health Publication No. 85-23,
revised 1985). The studies performed were carried
out according to the National Institutes of Health
Guide for the Care and Use of Laboratory Animals
and were approved by the local animal committee.
Induction of ischemic and reperfusion
injury.
The hepatic ischemia-reperfusion (I/R)
protocols were performed as described in a previous
study by Oleshchuk, 2012 [14]. There was no
mortality with this model. After the induction of
anesthesia (thiopentale sodium 20 mg/kg i.p.), the
liver of each rat was exposed through a midline
laparotomy. Complete ischemia of the median and
left hepatic lobes was produced by clamping the left
branches of the portal vein and the hepatic artery for
45
min. The right hepatic lobe was perfused to
prevent intestinal congestion. After the period of
ischemia, the ligatures around the left branches of
the portal vein and hepatic artery were removed. To
accurately evaluate the blood flow of the median
and left hepatic lobes after ischemia, the right
branches of the portal vein and the hepatic artery
were ligated to prevent shunting to the right lobe
after reperfusion and perfused for 2 h. The wound
was closed with 3.0 silk suture. Sham-operated
animals were similarly prepared except that no
ligature was placed to obstruct the blood flow to the
left and median hepatic lobes. Instead, the blood
flow to the right lobe of the liver was occluded. In
all groups rats were sacrificed after 1-h ischemia
followed by 3-h reperfusion. A total of 18 white rats
were equally divided into three groups (n=6 each
group). Group I (sham-operated control group) and
Group II (ischemia and reperfusion group) were
given 0.9% saline (1 mL/kg, i.p.) for 3 days. Group
III was pre-cotreated with L-arginine (25 mg/kg i.p.)
for 3 days before, last time 10min before induced
ischemia-reperfusion maneuver.
Peripheral blood and tissue procurement.
Blood sampling for determination of liver enzymes.
Blood samples were obtained from the right
ventricle via left anterior thoracotomy at the time of
sacrifice. Blood was collected in a sterile syringe
without anticoagulant and centrifuged at 2000 g to
separate the serum. The serum samples were stored
at −20°C until use for AST and ALT assays.

Protective effect of L-arginine on hepatic ischemia reperfusion injury: an experimental study
152
Проблемы биологии и медицины, 2014, №4.1 (81)
Blood sampling for cytokine and NOS
determination. Serum was removed from blood
samples by clotting for 2 hours on ice; serum was
centrifuged at 2,500×g (4
ο
C), filtered, aliguoted, and
frozen at −20°C until assayed for TNF-α, IL-1β, IL-
6, eNOS, and iNOS.
Small liver samples were collected from
each rat, than frozen immediately and stored in
liquid nitrogen until used for eNOS, and iNOS
assays.
Determination of liver enzymes function.
Determination of AST and ALT in plasma was
performed by Raytman-Frenkel method, using a
standard Kits "Filisit-diagnostic", Ukraine according
to the manufacture’s instruction. The activity of
AST and ALT in serum were expressed in mmol /
(L × h).
Cytokine assays.
For detection of TNF-α in
plasma,
a
specific
rat
Enzyme-linked
Immunosorbent Assay Kit E90133Ra Uscn Life
science inc. For rat interleukin 1 beta (IL-1β)
detection
in
plasma,
Enzyme-linked
Immunosorbent Assay Kit E90563Ra Uscn Life
science inc. For detection of rat interleukin 6 (IL-6)
in
plasma,
a
specific
Enzyme-linked
Immunosorbent Assay Kit E90079Ra Uscn Life
science inc.
NOS assays.
Determination of eNOS activity
and was performed by ELISA method using
«Enzyme-linked Immunosorbent Assay Kit for Rat
Nitric Oxide Synthase 3, Endothelial (NOS3)»,
Uscn, Life Science Inc, E90868Ra.
Determination of iNOS activity and was
performed by ELISA method using «Enzyme-linked
Immunosorbent Assay Kit for Rat Nitric Oxide
Synthase 2, Inducible (NOS2)», Uscn, Life Science
Inc, E90837Ra.
eNOS and iNOS expression was investigated
in blood plasma and liver tissue. Blood was
collected using EDTA as an anticoagulant. Samples
were centrifuged for 15 min at 1000 g/min at t 2-8
o
C
within 30 min after collection. Determination was
carried out immediately or frozen at t- 20
o
C.
The procedure liver cells lysis was performed
as follows:
1. Preparing liver homogenates on isotonic
NaCl at a ratio of 1:10.
2. Liver cells were centrifuged 5 min at 300 g,
the supernatant was then removed.
3. Cells were washed twice with isotonic
NaCl, after each wash was centrifuged at 300g 5
min.
4. By adding normal liver tissue lysis buffer
PBS (1 ml of buffer at 1×10
6
liver cells). It was
centrifuged 5 min at 300g.
5.
The
supernatant
was
collected.
Determination of enzyme activity was carried out
immediately or frozen at t- 20
o
C.
Determination
of
eNOS
and
iNOS
concentration were performed by ELISA method
and according to the he manufacture’s instruction.
eNOS and iNOS activity in serum expressed
as U/ml, hepatocytes expressed as U/g.
Histopathology study.
A portion of the tissue
from ischemic liver lobe was fixed in 10 % neutral-
buffered formalin solution for 5 days, embedded in
paraffin, and sectioned. The sections were stained
with hematoxylin and eosin.
Statistical analysis.
Statistical analyses were
performed by OriginPro Program. All data are
expressed as mean±standart devitation. Differences
between experimental groups were analyzed with an
unpaired 2-tailed Student
t
test. All differences were
considered statistically significant at a
p<0.05.
Results.
The results indicate that after 45
min ischemia followed by 2 h reperfusion the
activity of ALT in the blood increased from (0,44 ±
0,10) in the sham control group to (2,35 ± 0,09) in
animals with an I/R that is 5.3 times, increased AST
activity in accordance with (1,63 ± 0,12) h to (4,27
± 0,37), ie 2.6 times. The described dynamics
indicates that under simulated experimental injury
process cytolysis of hepatocytes is evolving (table
1).
The significant increase in ALT and AST
activities that occurred in the I/R group was
significantly suppressed by pre co-administration of
25 mg/kg L-arginine (Table 1).
Table 1.
Effect of L-arginine in activities of ALT and AST in the liver of sham and experimental groups of rat
Data
Sham (group 1)
I/R injury (group 2)
L-arginine +I/R (group 3)
ALT
0,44±0,10
2,35±0,09
р<0,001
1,10±0,09
р<0,005
р
1
<0,001
AST
1,63±0,12
4,27±0,37
р<0,001
2,83±0,20
р<0,01
р
1
<0,05
Results are expressed as mean±SD (n=6); Significantly different р – from sharm, р
1
– from I/R injury group;
activity of ALT and AST expressed in mmol/(l×h)

O. Oleshchuk
Биология ва тиббиёт муаммолари, 2014, №4.1 (81)
153
Thus, the enzyme activity of cytolysis were
significantly lower ALT (at 53.2%), AST (at 33.6
%). So, it was found that the prophylactic 3 days L-
arginine administration animals with IP improved
function of the liver.
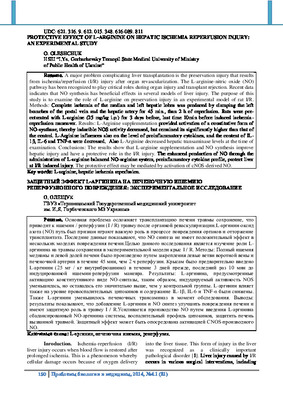
The results of the ELISA studies showed
significantly increased levels of proinflammatory
cytokines in the blood serum. Thus, the
concentration of IL-1β, IL-6 and TNF-α increased
respectively 8.8, 3.2 and 6.6 times in comparison
with the group 1 of animals (Figure 1).
In analyzing the impact of NO precursor L-
arginine in the level of proinflammatory cytokines
we found that the content of IL-1β, IL-6 and TNF-α
decreased by 38.9, 29.0, 33.9 % respectively.
*
**
*
**
*
**
0
10
20
30
40
50
60
70
80
90
pg/ml
IL-1
IL-6
TNF-α
sham
I/R
L-arginine+I/R
Figure 1: The content of proinflammatory cytokines in the serum of experimental animals: * – significantly
different from sham-operated group, ** – from I/R injury group.
Table 2.
eNOS and iNOS content in liver and blood of sham and experimental groups
Goups
blood
liver
eNOS
U/ml
iNOS
ng/ml
eNOS
oд./мл
(1 ml- 1×10
6
cells)
iNOS
нг/мл
(1 ml - 1×10
6
cells)
Sham
3,18±0,17
24,95±0,97
7,95±0,60
2,68±0,16
I/R
2,60±0,14
р<0,05
71,22±4,01
р<0,001
4,86±0,24
р<0,001
4,22±0,16
р<0,001
L–arginine
+I/R
3,50±0,24
р>0,1
р
1
<0,05
53,54±1,74
р<0,001
р
1
<0,001
6,98±0,17
р>0,1
р
1
<0,001
3,41±0,14
р<0,05
р
1
<0,001
Results are expressed as mean±SD (n=6); Significantly different р – from sharm, р
1
– from I/R injury group
Cytokines are potent inducers of iNOS,
whose content in the liver increased in 57.6 % and
in the serum – in 185.0 %. Unlike this, the
concentration of eNOS in the liver was reduced by
38.5 % and in the blood by 18.2 % compared with
the group 1 (table 2).
We observed one-way influence of the
substance on the contents of NO-synthase, both in
blood and in the liver. Enzyme immunoassay results
showed that the use of L-arginine in I/P leads to
increased eNOS content in hepatocytes (43.5 %) and
the reduction of iNOS (19.2 % ) (table 2).
At blood was observed a similar pattern.
Inducible NO-synthase was reduced by 24.8 % with
the introduction of L-arginine, but remained higher
than 2.1 times, compared with sham group of
animals. Endothelial isoform of the enzyme
increased by 34.5 % compared to its index in group
1.
Summarizing the above, we can say that
prophylactic co-administration of NO precursor L-
arginine before I/P is provided activation of a
constitutive form of NO-synthase, thereby inducible

Protective effect of L-arginine on hepatic ischemia reperfusion injury: an experimental study
154
Проблемы биологии и медицины, 2014, №4.1 (81)
NOS
activity
decreased,
but
remained
its
significantly higher than that of the control.
Discussion.
One of the criteria for liver
assessment in I/R experimental modelling is to
determine the activity in serum indicators cytolysis
of cells - enzymes ALT and AST. This study shows
significant activation in the I/R indicated enzymes,
which is consistent with the results of other
researchers [15]. This and previous our study
indicate
that
the
prophylactic
L-arginine
administration animals with IP has hepatoprotective
effect by inhibition of cytolisis [16].
It is an established fact that reactive oxygen
species and cytokines are potent inducers iNOS [16].
In this I/R study level of IL-1β, IL-6 and TNF-α in
I/R significantly increase, expression of liver iNOS
increased, eNOS level decreased. Our analysis of the
research results of other scholars showed that the
most pronounced hyperproduction of iNOS-
dependent NO occurs only after 4-6 hours after
onset of reperfusion, due to time-consuming
transcription and synthesis of the enzyme [17].
Therefore, in the early periods of reperfusion there is
lack of synthesis of NO, which may be due to
inhibition of еNOS [17]. Previously, we have found
that 2 hours of reperfusion levels of end products of
nitric oxide metabolism of nitrate does not change
significantly in the blood decreased in the liver, and
conversely decreased blood nitrite levels [16]. This
ratio NO
2
-
and NO
3
-
in the div can be explained by
the activation of nitrate and nitrate reductase cycle
(NO
3
-
→NO
2
-
→ NO
-
) under pathophysiological NO
failure at I/R. These data can be estimated as a
reduction total NO metabolites both in blood and
liver, which is confirmed by other researchers that
demonstrate the lack of NO at І/R [18]. We suggest
that NO deficiency is due not only to inhibition of
eNOS, but due to uncoupled of iNOS [20], which is
caused by high levels of ADMA at I/R [19], and
decrease of NO bioavailability in the early
reperfusion period [21].
I/R
is
characterized
by
changes
in
microcirculation, hypoxia, cytolysis and oxidative
stress in the liver [22]. NO donators and precursors
may improve microcirculation, suppress hypoxia,
cytolysis and oxidative stress.
Our previous studies have shown that the
application of L-arginine at І/R causes activation of
nitric oxide synthesis [16]. Increased concentrations
of NO stable metabolites nitrite and nitrate anion in
both blood and liver is consistent with our previous
and other scientists data [16, 23, 24].
We observed one-way impact on the content
of NO-synthase isoform in blood and in the liver.
The level of endothelial forms increased and
inducible – declined.
Increase in expression of endothelial nitric
oxide synthase in like circumstances recorded also
Rivera–Chavez F. A. et al., 2001 [25]. Therefore, we
can assume that the increase of nitric oxide synthesis
in the introduction of its precursors is due to
activation of constitutive forms NOS.
The mechanism of the protective influence of
precursor of nitric oxide synthesis in their care
administration, according to H. V. Markov,1996
[26], can be explained by the accumulation of
endogenous NO in the cells in a relatively stable
depot, which, if necessary, serves as an additional
source of endogenous nitric oxide. The mechanism
of the protective action of depot NO related on NO-
synthase inhibition on the principle of negative
feedback, or from disposing of excess active nitric
oxide. Perhaps this protective mechanism can
prevent the overproduction of NO and its related
cytotoxicity [27]. In addition, studies of P.
Chattopadhyay, 2010 showed that the protective
effect of arginine on functional status and
ultrastructure of liver in I/R connected with NO-
dependent reduction the Bcl-2 protein family
expression and thus inhibit the development of
necrosis and apoptosis of hepatocytes [24].
In conclusion, the enhanced production of NO
through the administration of L-arginine balanced
NO-arginine system, proinflamantory cytokine
profile, protect hepatobiliary system in liver I/R
induced injury. The protective effect may be
mediated by activation of cNOS-derived NO.
References:
1.
Chattopadhyay P. Protective effect of L–arginine
against
necrosis and apoptosis
induced
by
experimental ischemic and reperfusion in rat liver /
P. Chattopadhyay, G. Shukla, A. K. Wahi // The
Saudu J Gastroenterol. – 2009. – Vol. 15 (3). – P.
156–162.
2.
Vascular
occlusions
for
liver
resections.
Operative management and tolerance to hepatic
ischemia: 142 cases / E. Delva, Y. Camus, B.
Nordlinger [ et al.] // Ann. Surg
.
– 1989. – V. 209.
–
P. 211–218.
3.
Jaeschke H. Neutrophil and Kupffer cell-induced
oxidant stress and ischemia-reperfusion injury in rat
liver. / H. Jaeschke, A. Farhood // Am. J. Physiol.
–
1991. – V. 260. –
G. 355–362.
4.
Fan
C.
Therapeutic
approaches
for
ischemia/reperfusion injury in the liver / C. Fan,
R.M. Zwacka, J.F. Engelhardt // J Mol Med. – 1999.
– V. 77. – P. 577–596.
5.
Endothelial nitric oxide synthase protects the
post-ischemic liver: potential interactions with
superoxide / I.N. Hines, H. Harada, S. Flores [et al.]
// Biomed Pharmacother. – 2005. – V. 59. – P. 183–
189.

O. Oleshchuk
Биология ва тиббиёт муаммолари, 2014, №4.1 (81)
155
6.
Morris M. Recent advances in arginine
metabolism: roles and regulation of the arginases /
M. Morris // Br. J. Pharmacol. –
2009. – V.
157
. – P.
922-930.
7.
Morris M. Arginine Metabolism: boundaries of
our knowledge / M. Morris // J. Nutr. – 2007. – Vol.
137. – P. 1602–1609.
8.
Hirst D. G. Nitric oxide physiology and
pathology. / D. G. Hirst, T. Robson // Methods Mol
Biol. – 2011. – Vol. 704. – P. 1–13.
9.
Granger D. N. Nitric oxide: A modulator of
cell-cell adhesion and protein exchange in
postcapillary venules / Granger D.N., Kurose I.,
Kubes P. editors. // Shock, sepsis and organ failure-
nitric oxide. – Heidelberg Germany: Springer. –
1994. – P. 121–136.
10.
McCuskey R. S. Morphological mechanisms
for regulating blood flow through hepatic sinusoids /
R. S. McCuskey // Liver. – 2000. – V. 20. – P. 3–7.
11.
Ming Z. Nitric oxide mediates hepatic arterial
vascular
escape
from
norepinephrine-induced
constriction / Z. Ming, C. Han W. W. Lautt. // Am J
Physiol Gastrointest Liver Physiol. – 1999. – V. 277.
– G. 1200–1206.
12.
Squadrito GL, Pryor WA. Oxidative chemistry
of nitric oxide: The role of superoxide, peroxynitrite
and carbon dioxide / G. L. Squadrito, W. A. Pryor //
Free Radic Biol Med. – 1998. – V. 25. – P. 392–403.
13.
Phillips L. Nitric Oxide Mechanism of
Protection in Ischemia and Reperfusion Injury / L.
Phillips, F. Lopez–Neblina, L.H. Toledo–Pereyra // J
Invest. Sur. – 2009. – Vol. 22. – P. 46–55.
14.
Oleshchuk O. M. Experimental study of nitric
oxide precursors in hepatic ischemia-reperfusion / O.
M. Oleshchuk // Hospital surgery. – 2012. – N 4(60).
– P. 42–47. (in Ukraine).
15.
The impact of nitric oxide in ischemic pre-
conditioning of the liver in rats / Y.–Q. Zhan, X.–S.
Lu, Z.–M. Wang [et al.] // Zhopngguo putong waike
zazhi. – 2002. – Vol. 11, № 9. – P. 541–544.
16.
Oleshchuk O.M. Protective role of nitric oxide
in ischemia-reperfusion injury of the liver / O.M.
Oleshchuk // Pharmacology and Drug Toxicology. –
2010. – № 6 (19). – P. 41–45. (in Ukraine).
17.
Role of nitric oxide in liver ischemia and
reperfusion injury / I. N. Hines, S. Kawachi, H.
Harada [et al.] // Mol. and Cel. Biochemistry. –
2002. – № 234/235 – P.
229–237.
18.
Nitric oxide synthase distribution and expression
with ischemic preconditioning of the rat liver // R. S.
Koti, J.C. Tsui, E. Lobos [et al.] // FASEB J. – 2005.
– Vol. 19(9). – P. 1155–1157.
19.
Effect of simvastatin on nitric oxide synthases
(eNOS, iNOS) and arginine and its derivatives
(ADMA, SDMA) in ischemia/reperfusion injury in
rat liver / M. Trocha, A. Merwid–Lad, A. Szuba [ et
a.] // Pharmacological Reports. – 2010. – Vol. 62. –
P. 343–351.
20.
Increased inducible nitric oxide synthase and
arginase II expression in heart failure: no net
nitrite/nitrate production and protein S–nitrosylation
/ P. Heush, S. Aker, K. Boenger [et al.] // Am. J.
Physiol. Heart Circ. Physiol. – 2010. – Vol. 299. – P.
446–453.
21.
Role of endothelines and nitric oxide in hepatic
reperfusion injury in the rat / B. Pannen, F. Al–Adili,
M. Bauer [et al.] // Hepatology. – 1998. – № 27. –
P. 755–764.
22.
Oleshchuk
O.
M.
Prooxidant-antioxidant
balance at ischemic-reperfusion of liver of rats at the
presence of nitric oxide synthesis modulators / O. M.
Oleshchuk // Medical chemistry – 2012. – Vol. 6, №
2. – P. 49–53. (in Ukraine).
23.
Ploakanych
L. Y. The pathogenesis of liver
damage in ischemia-reperfusion her, involvement of
nitric oxide system / L. Y. Ploskanych, К. А.
Posokhova //
Achievements of Clinical and
Experimental Medicine. – 2008. – № 2– С. 138. (in
Ukraine).
24.
Chattopadhyay P. Protective effect of L–
arginine against necrosis and apoptosis induced by
experimental ischemic and reperfusion in rat liver /
P. Chattopadhyay, G. Shukla, A. K. Wahi // The
Saudu J Gastroenterol. – 2009. – Vol. 15 (3). – P.
156–162.
25.
Exogenous and endogenous nitric oxide but not
iNOS inhibition improves function and survival of
ischemically injured livers / F. A. Rivera–Chavez, L.
H. Toledo–Pereyra, R. E. Dean [et al.] // J. Invest
Surg. – 2001. – Vol. 14(5). – P. 267–273.
26.
Markov H. V. On bioregulatory system L-
arginine - nitric oxide / Х. В. Марков // Path.
physiology and exp. therapy. – 1996. – № 1. – P.
34–39 (in Russia).
27.
Hyperproduction of nitric oxide in the
pathophysiology of vascular. / J. К. Stokle, Б. Mulle,
R. Andriancitohayna [и др. ] // Biochemistry. –
1998. – № 7. –. 976–983 (in Russia).

Protective effect of L-arginine on hepatic ischemia reperfusion injury: an experimental study
156
Проблемы биологии и медицины, 2014, №4.1 (81)
REPERFUSION JAROHATLANISH
NATIJASIDA JIGAR ISHEMIYASIDA
L-ARGININNING HIMOYA TA’SIRI:
EKSPERIMENTAL TADQIQOT
O. OLESHCHUK
Ukraina SSV I.Ya. Gorbachevskiy nomidagi
Ternopol Davlat medetsina universiteti
Rezyume.
Bir yo'l organ zarar va naql rad
muhim rol o'ynaydi, deb organ revaskulyarizatsii.L-
arginin-nitrat oksidi so'ng ishemiya / reperfüzyon (I
/ R) jarohat olib keladi murakkablashtiruvchi jigar
transplant saqlash jarohati asosiy muammo (NO)
e'tirof etildi. Ekranga tomonidan ishlab chiqarilgan
edi jigar Full ishemiya vosita va chap lobları: Oxirgi
ma'lumotlar NO sintez bu o'rganish I / R. usullari
eksperimental irillagan modelida jarohati saqlash
bo'yicha L-arginin rolini tadqiq qilish uchun bo'ladi
zarar pecheni.Tselyu bir necha modellari hech ijobiy
ta'sirga ega ekanligini ko'rsatadi 45 daqiqa,
reperfüzyon kamida 2 soat davomida Portal ven va
jigar arteriyasi chap filiali. Rats ishemiyasi
reperfüzyon ogohlantirgandan manevra oldin oxirgi
10 daqiqa oldin 3 kun L-arginin (25 mg / kg i.p.)
oldindan qilingan. Natijalar: L-arginin, NO-sintazın
bir asoschilari aktivlashtirishni taqdim, shunday
indüklenebilir NOS faoliyat kamaydi, ammo bu
nazorat guruhiga nisbatan sezilarli darajada yuqori
bo'lib qoldi. L-arginin yallig'lanish tsitokinlari va
mazmuni IL-1β darajasini ta'sir, IL-6 va TNF-α
pasaytirildi. Bundan tashqari, L-arginin so'rov
o'tkazilgan paytda jigar transaminazalari kamaydi.
Xulosa: natijalar L-arginin qo'shilishi va NO sintez
jigar zarar yaxshilash va L-arginin Arginine NO-
muvozanatli tizimini, yallig'lanish sitokin tatbiq
tomonidan I / R.Usilivaetsya NO ishlab chiqarish
shikast himoya, bir o'rni bor, travma oqibatida jigar
himoya
ekanligini
ko'rsatadi.
Himoya
ta'siri
faollashtirish CNOS olingan hech vositachilik
mumkin.
Kalit so’zlar:
L-arginin, jigar ishemiyasi,
reperfusiya.